Conditions such as uterine fibroids, endometriosis, cancer of the; uterus, cervix, or ovaries, and uterine prolapse are most of the time painful and uncomfortable. Over the years treatment for these conditions has focused on the removal of the affected tissue or area. Still, the type of treatment is best decided when the patient and their physician consider what works well for the patient’s life style and statistics such as; survival rates, complications, recovery, and fertility.
Conditions such as uterine fibroids, endometriosis, cancer of the; uterus, cervix, or ovaries, and uterine prolapse are most of the time painful and uncomfortable. Over the years treatment for these conditions has focused on the removal of the affected tissue or area. Still, the type of treatment is best decided when the patient and their physician consider what works well for the patient’s life style and statistics such as; survival rates, complications, recovery, and fertility.
Surgeries and Assisting Tools
A hysterectomy is the removal of a woman’s uterus. It is a common procedure in the treatment of the conditions mentioned above. Generally this procedure is invasive and requires an abdominal incision. However, a smaller amount of women are now undergoing laparoscopic procedures which are minimally invasive surgeries that are performed by creating only a few very small incision sites. This is a convenient alternative for women who cannot afford a long recovery time.

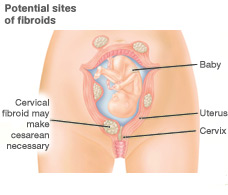
Another important procedure is a myomectomy, a technique used to remove uterine fibroids while leaving the uterus intact. This method of treatment can be done using either an invasive procedure or a laparoscopic tool. In addition to removing the fibroids embedded in the uterus, the surgeon must work to reconstruct the uterus.
Post-surgery it is important to help the body heal and prevent excessive scar tissue development. Too much scar tissue can become a painful experience and lead to further discomfort. Both Serrapeptase and Nattokinase are enzymes that have fibrinolytic activities that assist in the breakdown of fibrin and relieve inflammation by blocking chemical messages that trigger the inflammation cascade and any pain that may accompany it.
Proteases continue to assist the alleviation by breaking down cellular debris and toxins that could trigger increases in inflammation. Moreover, Nattokinase also works to break down scar tissue. These are all ideal for a speedy recovery and maintenance thereafter.
 One tool used for these laparoscopic surgeries is the power morcellator. This device is relatively small in size comprised of rotating blades for large tissue breakdown. After the large tissue has been fragmented, it is then vacuumed out of the area and faster than normal recovery time generally follows.
One tool used for these laparoscopic surgeries is the power morcellator. This device is relatively small in size comprised of rotating blades for large tissue breakdown. After the large tissue has been fragmented, it is then vacuumed out of the area and faster than normal recovery time generally follows.
Possible complications
Despite this type of tool being favored for many years, it has recently been a topic of concern for its few accompanying cases involving metastasis of cancerous cells that were left behind during these procedures. In most affected women, undetected cases of early stage cancer were in the area of focus during surgery. If any of the cancerous cells are left behind, they spread to other areas of the body turning the cancer from a very treatable stage into its deadliest stage.
While this resulting complication may be relatively low in occurrence, spreading of uterine cancer found in 1 out of 350 women, the concern is high.
New methods and Improvements
Finding solutions to serious complications such as these are highly important for both the patient and surgeon. It is both extremely stressful and frustrating to go in to treat one condition and come out to find another, much worse, has invaded your body. Hysteroscopy is one improvement to the laparoscopic technique also known as open morcellation.
The procedure of Hysteroscopy, closed morcellation, consists of fragmenting the tissue and collecting it into pouches. With mechanical maneuvering it facilitates the surgeon’s job by providing full control over the cutting and collecting of the tissues. Currently this alternative seems promising but, further studies must be continued to ensure there is no correlation between the technique and the spreading of cancerous cells.
With any procedure, following its protocols and guidelines will almost always yield the desired results. Hysteroscopy already is a step in the right direction, provided its benefit of decreasing the possibility of spreading cancerous tissue,. Additionally, any tissue collected in the tissue pouches can be used to complete further testing assisting in the detection of existing sarcoma cells.
 Women who have to deal with fibroids know that managing levels of the hormone estrogen and progesterone is very important. Most prescribed medication deals around this issue since it has been suggested fibroids growth may be linked to a high estrogen and progesterone setting. As they grow the symptoms that accompany them are more pronounced. Pain, heavy bleeding, and inflammation are common results of these and can possibly lead to other underlining issues. However, most women with uterine fibroids do not experience any symptoms. It is likely for women who do have heavy or in between period bleeding, to develop an iron deficiency. While in others fibroids may cause a very painful period but, in some cases this pain could also be a result of endometriosis. When tissue that lines the uterus grows in other areas it is known as Endometriosis, this tissue breaks down and causes bleeding during menstruation. Following the tissue breakdown scar tissue develops in the areas it has grown in, this leading to a painful period.
Women who have to deal with fibroids know that managing levels of the hormone estrogen and progesterone is very important. Most prescribed medication deals around this issue since it has been suggested fibroids growth may be linked to a high estrogen and progesterone setting. As they grow the symptoms that accompany them are more pronounced. Pain, heavy bleeding, and inflammation are common results of these and can possibly lead to other underlining issues. However, most women with uterine fibroids do not experience any symptoms. It is likely for women who do have heavy or in between period bleeding, to develop an iron deficiency. While in others fibroids may cause a very painful period but, in some cases this pain could also be a result of endometriosis. When tissue that lines the uterus grows in other areas it is known as Endometriosis, this tissue breaks down and causes bleeding during menstruation. Following the tissue breakdown scar tissue develops in the areas it has grown in, this leading to a painful period.